Posterior Urethral Valve--- A Radiological Interpretation by RGU and MCU
Sajjad Ahmad Dar1, Arsheed Iqbal2, *, Imran Nazir Salroo4,
A. Rashid3, Afroza Jan2, Amjed Waheed5
1Head of the Department of Radiodiagnosis and Imaging, Govt. Medical College, Facility of Radiology, University of Kashmir, Srinagar (J&K) India
2Regional Research Institute of Unani Medicine, Ambedkar University Faculty of Unani Medicine, Department of Central Council for Research in Unani Medicine, Srinagar (J&K), India
3Govt Medical College, Department of Urology, Faculty of Surgery, University of Kashmir, Srinagar City, Jammu and Kashmir, India
4Department of Radiodiagnosis and Imaging, Govt. Medical College, Facility of Radiology, University of Kashmir, Srinagar (J&K) India
5Medical Officer, Directorate of ISM, Hamdard University Faculty of Medicine, New Delhi, India
Email address

(A. Iqbal)
*Corresponding author
Citation
Sajjad Ahmad Dar, Arsheed Iqbal, Imran Nazir Salroo, A. Rashid, Afroza Jan, Amjed Waheed. Posterior Urethral Valve--- A Radiological Interpretation by RGU and MCU. International Journal of Chemical and Biomedical Science. Vol. 2, No. 6, 2016, pp. 42-46.
Abstract
Posterior Urethral Valve: (PUV): Is an obstructive developmental anomaly in the urethra of male new born [1] is the commonest and is the commonest cause of lower urinary tract obstruction in male infants. In the present era the most common mode of presentation is antenatal diagnosis. Postnatally, PUV can have a broad spectrum of presentations ranging from a life threatening pulmonary hypoplasia due to oligohydramnios, to mild obstruction or symptoms that may escape early detection and manifest only in later childhood, adolescence or even adulthood. Universally accepted treatment protocol for managing PUV includes cystoscopic valve ablation using cold knife or electrocautery or LASER. The disorder varies in degree and the very mild as the severe cases can have renal and respiratory failure from lung under development as a result of low amniotic fluid volumes etc. [2] Posterior Urethral Valve presents the most common aetiology of congenital urethral obstruction in young boys and the most common urologic causes for and stage renal disease in children the incidence of (PUV) is one in 8000 babies [3] It comprises 10% of all parentally diagnosed uropathies and occurs approximately 1:4000 live male births.
Keywords
Urethra, Cystoscopy, Valve, Urogenital
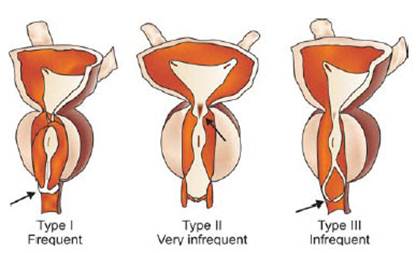
1. Types of Posterior Urethral Valve
These are following three type of (PUV).
Type I - Most common type; due to anterior fusing of the plicaecolliculi, mucosal fins extending from the bottom of the verumontanum distally along the prostatic and membranous urethra [4]
Type II - Least common variant; vertical or longitudinal folds between the verumontanum and proximal prostatic urethra and bladder neck.
Type III - Less common variant; a disc of tissue distal to verumontanum, also theorized to be a developmental anomaly of congenital urogenital remnants in the bulbar urethra.
The congenital urothelial remnants of type III posterior urethral valves have been referred to as COBB’s Collar or Moorman’s ring [5]
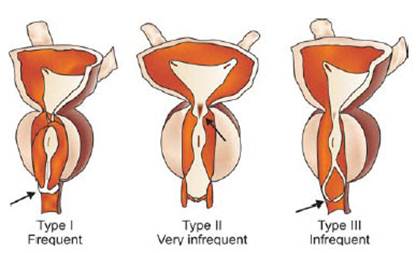
Figure 1. Showing different types of posterior urethral valve.
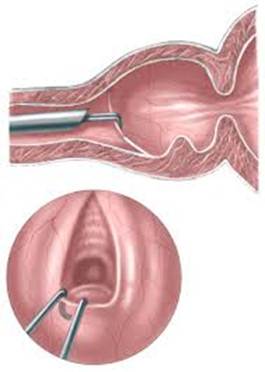
1.1. Voiding Cystourethrogram(VCUG)
Voiding Cystourethrogram (VCUG) is more specific for the diagnosis. PUV on voiding cystourethrogram is characterised by an abrupt tapering of urethral calibre near the verumontanum, with the specific level depending on the developmental variant vesicoureteral reflux is also seen in over 50% of cases. Diagnosis can also be made by cystoscopy the treatment is by endoscopic valve ablation. Specific procedures for in utero interrention include infusion of amniotic fluid, serial bladder aspiration, and creating a connection between the amniotic sac and the fetal bladder, or vesicoamniotic shunt [6] the standard treatment is primary ablation of the valves [7] urinary division is under in used in selected cases [7] and its benefit is disputed [8][9]
1.2. Pathophysiology and Long Term Outcome
An abnormal confluence of the mesonephric duct with the Urogenital sinus membrane during the 7th week of gestation, results in the valvular urethral obstruction of the posterior urethra.
The earlier the obstruction the more severe is it consequence. This implies that there is a spectrum of clinical severity in patients with posterior urethral valves. At the extreme end of this spectrum is a severe obstruction, with arrested renal development, oligohydroamnios and pulmonary dysplasia, which in clinical practice translate intospontaneous abortion or neonatal death. Neonates with underdeveloped kidneys but well-developed lungs, who survive the neonatal period, still have 20-30% risk of progression to the end stage renal failure in the first decade of life [11].
The majority of PUV patients of all groups have a degree of incontinence. This is initially related to the uninhibited detrusor contractions and reduced bladder capacity.
Later in life, particularly after puberty, when the bladder capacity increases, the incontinence can be related to the hypocontractile detrusor and large post void residuals [12].
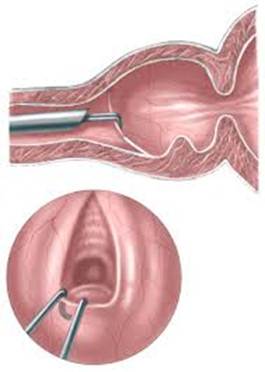
Figure 2. Showing the valve position in PUV.
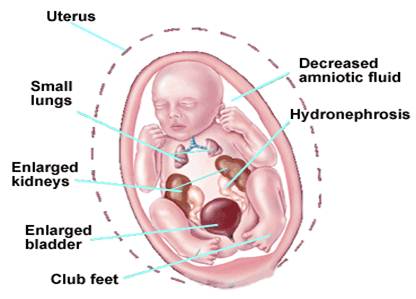
1.3. Prenatal
The diagnosis of posterior urethral valve in prenatal period is made by ultrasonography. Up to 80% of patients are diagnosed prenatally. The most severe obstruction with dilatation of the urinary tract may be detected as early as the 14th week of gestation. Half of the PUV doetuses are picked up before the second trimester scan.
The heightened awareness of the condition implies that virtually any male foetus with bilateral hydronephrosis assumed to have posterior urethral valves until proven otherview. In addition to this concept there are some ultrasonographic features of posterior urethral valves that help in diagnosis and prediction of the severe cases.
The persistently distended foetal urinary bladder with the keyhole signis highly suggestive of PUV [13]. The gestational age at the detection of PUV before the 24th week, the thickened bladder wall, the hypergenicity of the renal parenchyma and oligohydramnios are all features predictive of poor renal function with an early onset of renal failure [10].
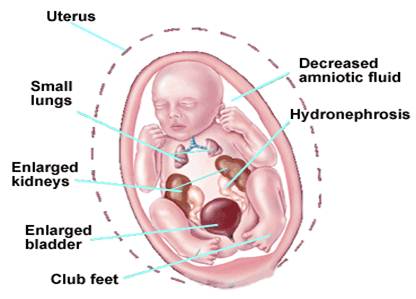
Figure 3. As labled above.
1.4. Neonatal
The neonatal presentation can be related to the effects of impaired renal function: poor feeding, listlessness, and irritability. Less commonly parents or careers pick up a poor urinary stream. Even less common is the urinary as cites that that develops as a pop off mechanism in severe form of valvular obstruction.
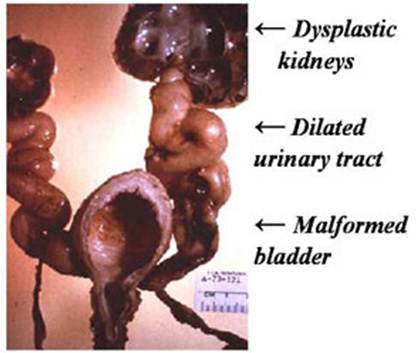
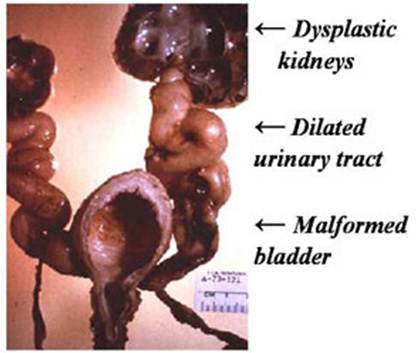
Figure 4. Showing the complications in bladder urethra and kidneys in chronic posterior urethral valve patient.
1.5. Presentation in Infancy
The presentation of PUV in the first year of life is mostly related to the urinary tract infections and urinary sepsis. Other signs include abdominal distension, palpable bladder or kidneys, poor urinary stream, urinary dribbling, failure to thrive or poor feeding.
1.6. Late Presentation
Fifty per cent of boys with PUV over five year of age present with urinary incontinence or enuresis [14], and shows complications like dysplastic kidneys, dilated urinary tract. malformed bladder and at times more severe problems in genitourinary system.
1.7. Ultrasonography
Both in prenatal and postnatal period, posterior urethral valves can be suspected in the presence of bilateral hydronephrosis with uretric dilatation associated with increased thickness of the bladder wall, hyperechoic renal parenchyma and increased post void residuals (in older boys). All boys with suspected posterior urethral valves should undergo maturating cytsourethrogram. Following pictures revealsthe said changes.- Fig 1 to Fig 4

Figure 5. Showing hydronephrosis in posterior urethral valve case.

Figure 6. Showing hydronephrosis in posterior urethral valve case with thinning of cotex.

Figure 7. Shows hydroureteronephrosis in posterior urethral case.
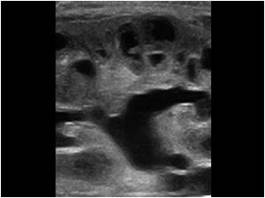
Figure 8. Shows dilated pelviccalyceal system with increased cortical echotexture in chronic posterior urethral case.
1.8. Micturating Cystourethrogram
This remains a gold standard for the diagnosis of urethral valves. On Cyst urethrogram the posterior urethra is always dilated and elongated. Some patients with severe obstruction regurgitate the contrast into the ejaculatory ducts and spermatic vesicles. The bladder neck is usually clearly demarcated. The urinary bladder wall is thickened with different degree of trabeculation and pseudodiverticulae.27-55% of patients with PUV also have vesico-ureteric reflux [10]. Following figures (Fig 5 and Fig 6) reveals accurately the picture of posterior urethral valve on micturatingcystourethrogal.

Figure 9. Shows clear demarcation of posterior urethral valve on micturatingcystourethrogram.

Figure 10. Shows more established case of posterior urethral valve on micturatingcystourethrogram.
1.9. Differential Diagnosis
Obstruction of the male urethra can also be caused by rare conditions, such as anterior urethral valves, urethral diverticulum and syringocele. Urethral diverticulum is located at the level of peno-scrotal junction and presents with post micturitional dribbling or urinary tract infections. Cowper's gland cyst or syringocele is usually presented with post micturitional dribbling in older boys. Generally, saccular lesions of the male urethra may occur anywhere along the penile urethra including the fossa navicularis. Their presentation varies from mild obstructive symptoms to recurrent urinary tract infections and sometimes stone formation within the diverticulum.
2. Discussion
The most common cause of bladder outlet obstruction in boys is posterior urethral valve. Various treatment options are available for managing cases with PUV, most voidly accepted being the valve ablation. [15], [16], [17] Posterior urethral stricture is considered the most debilitating because, if not managed properly, may lead to severe impairment of the quality of life, by affecting continence and potency.
PUV is seven times more common than AUV; however, the obstructive effects of AUV can be equally dam- aging. The association of AUV and PUV could not be explained on an embryological basis as the source of AUV and PUV development is different. The etiology of AUV is still controversial, but faulty union of the glandular and penile urethral segments, in-complete formation of the corpus spongiosum, congeni-tal cystic dilation of the per-urethral glands, and abortive attempt at urethral duplication have been proposed as possible mechanisms. [18], [19], [20] AUV can be located anywhere distal to the membra-nous urethra and, in terms of distribution; these valves are most common in the bulbar urethra (40%) [18], [19], [21]
The clinical manifestation of AUV and PUV is highly variable and depends on patient age and degree of obstruction. It may range from minimal obstruction to se-vere obstruction with bilateral severe hydroureteroneph-rosis, end-stage renal disease, and even bladder rupture [18], [19], [22], [23]. Physical examination findings can be normal. Prenatal ultrasonography may suggest the diagnosis of AUV and PUV through visualization of urethral dilata- tion and hydronephrosis, oligohydramnios and bladder distension highly suggestive of infravesical obstruction. Cystourethrography is the mainstay of the diagnosis. It can reveal a thickened trabeculated bladder, a dilated or elongated posterior urethra, a dilation of the anterior urethra, and a hypertrophied bladder neck. Diverticula and vesicoureteral reflux may also be present. The spectrum of severity of AUV ranges from mild urethral dilatation to bilateral hydronephrosis with renal insufficiency (Figure 3) [24, 25]. There are various treatment methods such as open ure-throtomy and excision of the valve, segmental urethrectomy of the valve-bearing area along with a primary end- to-end anastomosis, cold disruption and transurethral resection of the valve. But endoscopic valve ablation by electrocautery has been the procedure of choice. In our case the endoscopic resection gave good results after 6 months of follow up.
3. Results
In the present study 3000 patients were screened over a period of about six years for urinary tract ailments and out of it 1100 cases were clinically symptomatic and sent for radiological investigations viz., MCU and RGU for evaluation of anterior urethal valve. Out of 1100 cases, 57 subjects were confirmed with anterior urethral value as confirmed by MCU and RGU (Figure 1). In the present study the sensitivity of RGU and MCU could be established in the diagnosis of this disease. Further the rear nature of this disease is established as only 5.18 % of the subjects were radiologically diagnosed for anterior urethral valve.
4. Conclusion
Posterior urethral valve is the anomaly found in the urinary tract of male children with quit higer incidence rate than anterior urethral valve and is diagnosed radiologically by RGU and MCU, however other investigations are also of paramount importance but here in this studythe diagnosis was done by RGU and MCU.
References
- Manzoni C, Valentini A (2002). "Posterior urethral valves." Rays 27 (2): 131–4. PMID 12696266.
- "Emedicine - Posterior urethral valves - overview and treatment.". Emedicine. Retrieved July 26, 2010.
- "Posterior urethral valves - Disease Information.". Children's hospital, Boston. Retrieved January 31, 2011.
- "Nationwide Children's Hospital, Radiology - Posterior urethral valves". Nationwide Children's Hospital. Retrieved July 26, 2010.
- "Nationwide Children's Hospital, Radiology - Cobb's Collar". Nationwide Children's Hospital. Retrieved July 26, 2010.
- "Emedicine - Posterior Urethral Valves - Diagnosis and Treatment". Emedicine. Retrieved July 18, 2010.
- Warren J, Pike JG, Leonard MP. Posterior urethral valves in Eastern Ontario - a 30 year perspective. Can J Urol. 2004 Apr;11(2):2210-5. PMID 15182412.
- Kim YH, Horowitz M, Combs A, Nitti VW, Libretti D, Glassberg KI. Comparative urodynamic findings after primary valve ablation, vesicostomy or proximal diversion. J Urol. 1996 Aug;156(2 Pt 2):673-6. PMID 8683757.
- Smith GH, Canning DA, Schulman SL, Snyder HM 3rd, Duckett JW. The long-term outcome of posterior urethral valves treated with primary valve ablation and observation. J Urol. 1996 May;155(5):1730-4. PMID 8627873
- Hutton, K. A., Thomas, D. F., Arthur, R. J et al. Prenatally detected posterior urethral valves: is gestational age at detection a predictor of outcome? J. Urol. 1994.
- Parkhouse H, Barratt TM, Dhillon MJ et al. Long Term outcome of boys with posterior urethral valves. Br J Urol 1988; 62: 59-62.
- Holmdahl G, Sillen U, Hanson E et al. (1996) Bladder dysfunction in boys with posterior urethral valves before and after puberty. J Urol 155:694-8.
- Mahoney BS (1994) Ultrasound evaluation of the fetal genitourinary system. In Callen PW(ed) Ultrasonography in obstetrics and gynecology. 3rd edition. Philadelphia, PA: WBSaunders, 400-10.
- Williams DI, Whitaker RH, Barratt TM et al. Urethral Valves. Br J Urol 1973; 45:200-210.
- Farhat W, McLorie G, Capolicchio G, Khoury A, Bägli D, Merguerian PA. Outcome of primary valve ablation versus urinary tract diversion in patients with posteriorurethral valves. Urology 2000;56:653-7.
- Walker RD, Pardon M. The management of posterior urethral valves by initial vesicostomy and delayed valve ablation. J Urol 1990;144:1212-4.
- Yohannes P, Hanna M. Current trends in the management of posterior urethral valves in the paediatric population. Urology 2002;60:947-53.
- Bhagat, S. K., Gopalakrishnan, G., Kekre, N. S. and Ku-mar, S. (2008) Anterior and posterior urethral valves with subcoronal hypospadias: A rare association. Journal of Pediatric Surgery, 43, E23-E25.
- Kajbafzadeh, A. M., Jangouk, P. and AhmadiYazdi, C. (2005) Anterior urethral valve associated with posterior urethral valves. Journal of Pediatric Urology, 1, 433-435. doi:10.1016/j.jpurol.2005.05.007
- McLellan, D. L., Gaston, M. V., Diamond, D. A., Lebovitz, R. L., Mandel, J., Atala, A., et al. (2004) Anterior urethral valves and diverticula in children: A result of ruptured Cowper’s duct cyst. British Journal of Urology Interna-tional, 94, 375e8.
- Kibar, Y., Coban, H., Irkilata, H. C., Erdemir, F., Seckin, B. and Dayanc, M. (2007) Anterior urethral valves: An uncommon cause of obstructive uropathy in children. Journal of Pediatric Urology, 3, 350-353.
- Firlit, C. F. and King, L. R. (1972). Anterior urethral val- ves in children. Journal of Urology, 108, 972e6.
- Aygün, C., Güven, O., et al. (2001) Anterior valve as a cause of end stage renal disease. International Journal of Urology, 8, 141-143. doi:10.1046/j.1442-2042.2001.00270.x
- Narashiman, K. L., Choudhary, S. K. and Kaur, B. (2005) Anterior urethral valves. Indian Pediatrics, 42, 708-710.
- Bhagat, S. K., Gopalakrishnan, G., Kekre, N. S. and Ku- mar, S. (2008) Anterior and posterior urethral valves with subcoronal hypospadias: A rare association. Journal of Pediatric Surgery, 43, e23-e25. doi:10.1016/j.jpedsurg.2008.04.026

 (A. Iqbal)
(A. Iqbal)